Introduction: The Challenge of Funding A&E Services
Accident and Emergency (A&E) departments in the NHS are under constant pressure. Every year, millions of patients turn up at A&E – and the numbers have been rising. In England, major A&E units (the 24-hour consultant-led departments) saw 16.5 million attendances in 2023/24, about 2.6 million more than in 2010/11. That’s a huge increase in people needing urgent care. Planning the budget to run these services is a tricky balancing act. If planners allocate too little money, departments can become overstretched – leading to overcrowded waiting rooms and missed targets. Allocating too much might seem unlikely given tight NHS finances, but over-budgeting could mean funds not used optimally elsewhere. How can we get this balance right, especially when demand can swing unpredictably?
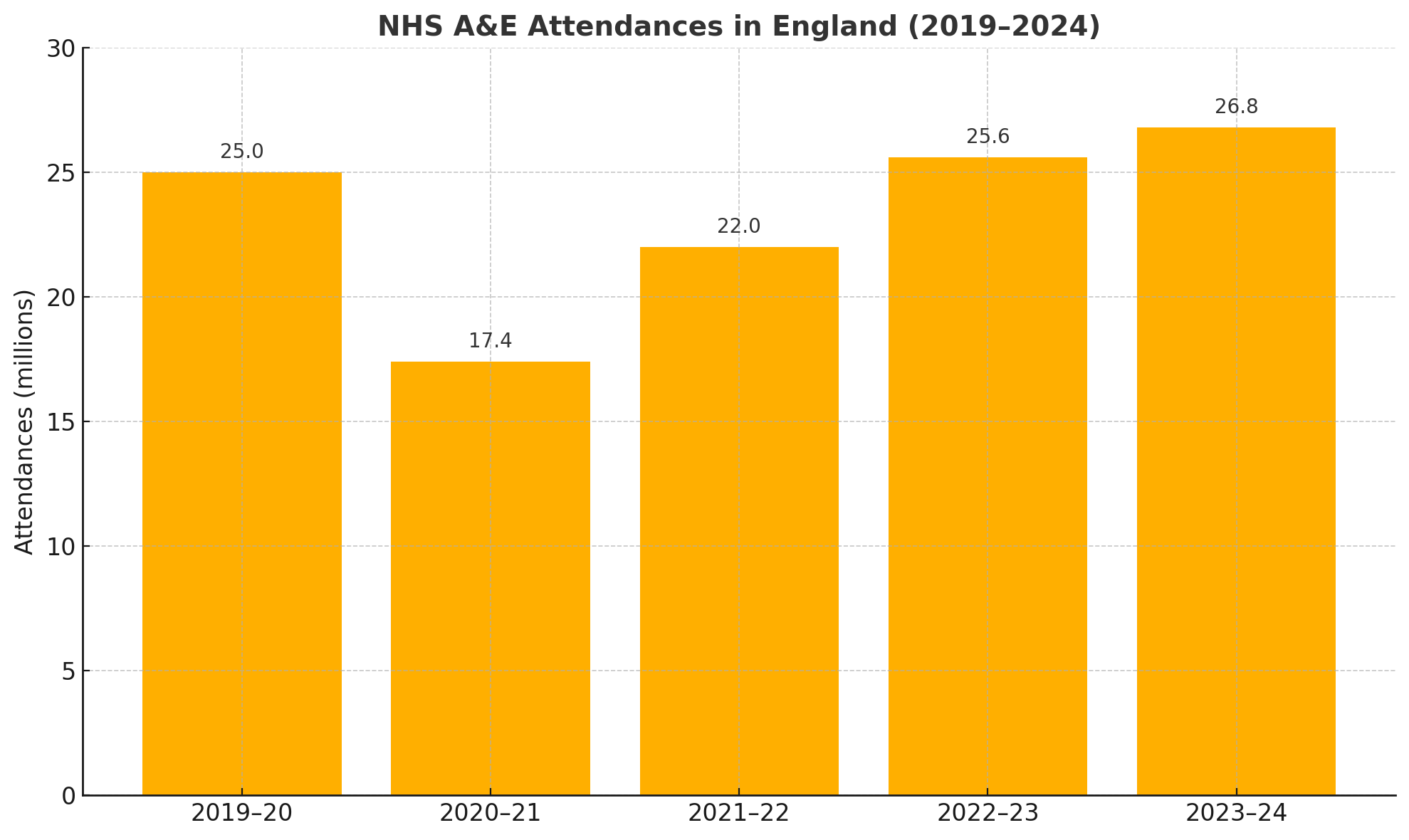
To appreciate the challenge, consider how unpredictable A&E demand can be. The COVID-19 pandemic illustrated this dramatically. In April 2020, during the first lockdown, A&E attendances plummeted by almost 50% compared to April 2019 as people avoided hospitals. Yet by 2023, attendances had not only rebounded but hit record levels, returning to pre-pandemic trends of growth. This variability makes traditional budgeting (often based on last year’s figures or fixed targets) a risky proposition.
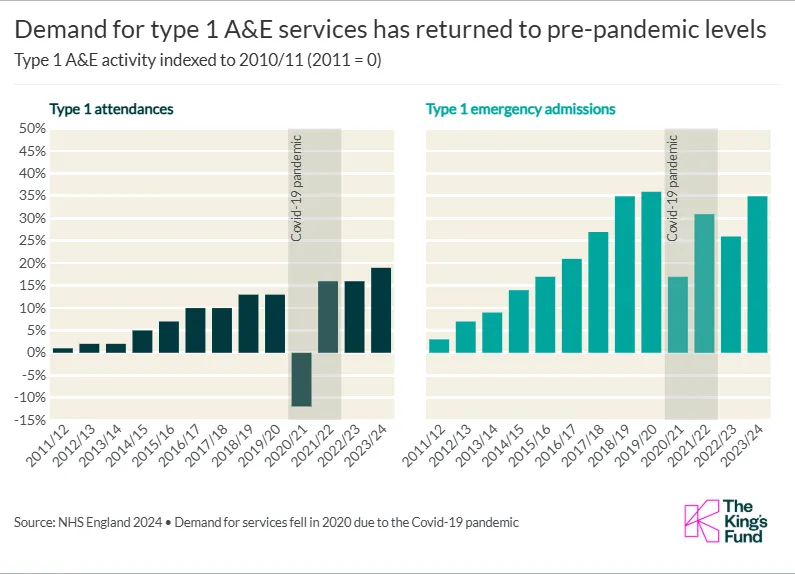 A chart showing the rise, fall, and rebound in A&E attendances and emergency admissions from 2011 through 2023/24, indexed to 2010/11. The dramatic dip in 2020/21 corresponds to the Covid-19 pandemic, followed by a strong recovery by 2023/24. This visual highlights both the upward long-term trend in A&E demand and the significant year-to-year volatility.
A chart showing the rise, fall, and rebound in A&E attendances and emergency admissions from 2011 through 2023/24, indexed to 2010/11. The dramatic dip in 2020/21 corresponds to the Covid-19 pandemic, followed by a strong recovery by 2023/24. This visual highlights both the upward long-term trend in A&E demand and the significant year-to-year volatility.
Healthcare leaders are increasingly looking for smarter tools to guide decisions. One such tool borrowed from statistics and economics is Bayesian Decision Theory. In simple terms, Bayesian methods incorporate uncertainty and new evidence into decision-making. This article will explain how Bayesian decision-making could improve A&E budget planning – using plain language and real data. We’ll compare it to traditional budgeting approaches, explore examples of probabilistic thinking in managing emergency care, and show how the NHS’s rich historical data can feed into predictive models. The goal is to show an interested but non-expert reader that, while the term sounds complex, Bayesian Decision Theory is essentially about making informed decisions when you’re uncertain – a daily reality in NHS budgeting.
Traditional A&E Budget Planning vs. a Bayesian Approach
How budgets are set today: Typically, NHS budgets for A&E (and other services) are planned on an annual cycle. Each year, the Department of Health and Social Care allocates funds to NHS England, which then passes money to regional bodies (now Integrated Care Boards) and hospital trusts. Planners look at factors like last year’s spending, projected patient numbers, government priorities and specific targets (for example, the A&E 4-hour wait target) to decide how much funding A&E departments will get. This process often relies on deterministic estimates – essentially single “best guess” numbers for next year’s demand and costs. For instance, a trust might assume A&E attendances will increase by, say, 2% next year and budget accordingly. In practice, this can become an incremental exercise: last year’s budget plus a bit more (or a required efficiency saving), adjusted by known factors like inflation or planned new services.
The traditional approach has some drawbacks. Surprises can and do happen. A bad flu season, a heatwave, or unforeseen events like pandemics can send attendance numbers far above (or below) predictions. When that happens, hospitals either scramble to find emergency funds or end up overspending. In fact, local NHS systems in England overspent by a combined £1.4 billion in 2023–24, more than double the previous year’s deficit, largely due to rising demand and other pressures. That overspend occurred despite billions in extra funding injections, indicating how hard it is to get the budget right when circumstances change rapidly. Traditional budgeting often isn’t flexible enough to adapt once the year is underway – money is largely fixed in advance, and adjusting it is difficult.
What a Bayesian approach offers: Bayesian Decision Theory provides a framework to plan under uncertainty. Instead of treating the future as one fixed forecast, a Bayesian approach treats it as a range of possible outcomes, each with a certain probability. In practical terms, this means acknowledging “we don’t know exactly what will happen, but here are the odds of various scenarios.” Planners can then allocate resources in a way that, on balance, works best across all those possibilities.
For example, imagine planning A&E services for an upcoming winter. A traditional plan might budget for an averagewinter. A Bayesian-inspired plan would consider multiple scenarios: perhaps a 20% chance of a mild winter (lower A&E attendances), a 50% chance of a normal winter, and a 30% chance of a severe winter (e.g. a big flu outbreak causing a surge in emergency patients). Each scenario has a probability attached. Bayesian Decision Theory says we should weigh decisions against these probabilities and the costs/benefits of each outcome. In other words, it’s about maximising expected utility – choosing the action that gives the best overall result when considering all the what-ifs. In this context, “utility” could be thought of as achieving good patient care within budget without crises. The optimal decision might be, for instance, to earmark some extra contingency funding or to schedule additional staff just in case if the risk of a surge is high – even though that surge is not guaranteed. Traditional budgeting might balk at spending money on a surge that “might not” happen, whereas a Bayesian planner would justify it by the calculated risk. Essentially, Bayesian planning builds a safety margin informed by data: if the chance of a severe event is significant, the plan accounts for it proportionally.
Another difference is that Bayesian methods encourage continual updating. Rather than set a budget in stone and forget it, a Bayesian-minded approach would update projections as new data comes in. Suppose mid-way through the year, A&E attendances are trending much higher than expected. A Bayesian framework would formally incorporate that new evidence and could trigger pre-planned adjustments – maybe activating reserve funds or other measures that were contingent on the data crossing a certain threshold. (In real NHS finance processes, this could translate to in-year reviews or requests for additional support if certain triggers are met.) It’s a bit like how meteorologists update a weather forecast when new information arrives; similarly, health planners could update their “forecast” for demand and costs. Traditional budgeting doesn’t always do this until it’s too late, whereas a Bayesian approach embraces updating as a principle.
Bayesian Decision Theory in Plain Language
So what exactly is Bayesian Decision Theory, in everyday terms? At its heart, it’s a method for making decisions when you’re uncertain by using probability. It’s named after Thomas Bayes, an 18th-century minister and statistician, but don’t worry – you don’t need to do any complicated maths here. The key idea is pretty intuitive:
- Start with what you know (or think you know). You have some prior beliefs or data. For example, historically you know roughly how many patients usually come to A&E each month, and how much it costs to treat them. You might also have prior knowledge like “winters are usually busier than summers” or “during school holidays, attendance dips slightly,” etc.
- Update with new evidence. As new information comes in, you update your expectations. Perhaps you hear that a new strain of virus is spreading, or the early winter has been colder than average – this might increase the likelihood of a busy A&E period. Bayes’ Theorem is the mathematical rule that tells us how to adjust the probabilities of outcomes given new evidence. In simple terms, it’s a formula for learning from experience. If the evidence suggests a surge is more likely, our model’s probability for that scenario goes up.
- Consider the cost and benefit of decisions under each outcome. Bayesian Decision Theory isn’t just about predicting; it’s about deciding. For each possible scenario, you think about the consequences. For instance, “If I allocate an extra £5 million to A&E and a surge happens, was that enough to handle it? If a surge doesn’t happen, what’s the opportunity cost – could that money have been better used elsewhere?” Each decision (allocate more funds, hold steady, etc.) will have a result under each scenario (surge or no surge), and some results are better than others.
- Pick the decision that gives the best balance on average. This is the expected utility idea. Essentially, for each decision you weigh outcomes by their probability. A decision that might be slightly more costly in one scenario could be worth it because it averts a disaster in a more likely scenario. Bayesian decision-making will favor the choice that has the highest weighted benefit when you consider all the scenarios and their odds. It’s like placing bets with the odds in mind – you’re not going all-in on one guess of the future, you’re hedging in proportion to what’s likely.
In plainer terms, Bayesian Decision Theory helps answer questions like: “Given what we know, what’s the smartest plan, knowing we could be wrong?” It’s a formal way to do what-if planning. Humans do a rough version of this all the time (“Should I bring an umbrella? The forecast says 30% chance of rain, I’ll risk it or I won’t, based on my tolerance for getting wet”). In the NHS A&E context, it might translate to: “Should we open an extra temporary ward this winter? There’s, say, a 1 in 3 chance we’ll desperately need those beds. Is it worth the cost even if there’s a 2 in 3 chance they won’t be fully used?” A Bayesian approach frames this decision clearly by quantifying those chances and potential consequences.
Another aspect of Bayesian thinking is that it allows for expert judgement and data to work together. Planners can start with educated guesses (priors) and then refine them with actual data. For example, clinical and management staff might feel that “summers are getting busier in A&E nowadays” – Bayesian methods would incorporate historical data to either confirm this trend or not, updating the beliefs. Over time, as more data becomes available (for instance, each month’s attendances, or new research on population health), the decisions improve. Bayesian Decision Theory, in short, is a way to formalize common sense with the help of math: be prepared for various outcomes, lean more towards what’s likely but don’t ignore the less likely events if they would have big impacts.
Feeding the Model: Using NHS Data and Trends
One reason Bayesian approaches are so promising for NHS budgeting is that the NHS sits on a treasure trove of data. Every A&E attendance, every admission, every seasonal trend – it’s all recorded. Historical datasets from NHS England show how A&E demand has changed year by year, and even week by week. By tapping into this rich history, we can better forecast and prepare for the future.
Let’s look at some real NHS A&E data to see what we have to work with. Table 1 below shows the total number of A&E attendances in England in recent years, illustrating the trend and the impact of the pandemic:
| Year (Financial Year) | Total A&E Attendances (England) |
|---|---|
| 2019–20 (pre-pandemic) | 25.0 million |
| 2020–21 (pandemic year) | 17.4 million |
| 2023–24 (post-pandemic) | ≈26.8 million |
Table 1: Total annual attendances at NHS A&E departments in England. The COVID-19 pandemic caused a sharp drop in 2020/21, but by 2023/24 demand not only recovered but slightly exceeded pre-pandemic levels.
This data highlights a few important points for a Bayesian model:
- Long-term growth: Demand has generally trended upwards (2019/20 saw far more attendances than a decade earlier). This can be built into the “prior” expectation that, all else equal, next year will likely be a bit busier than last.
- Variability and shocks: The huge dip in 2020/21 (a 30% fall) was an extraordinary event. While we hope not to see a repeat of a pandemic, it shows that rare but major disruptions are possible. A Bayesian approach doesn’t dismiss such outliers – instead, it can incorporate them as low-probability but high-impact scenarios (sometimes called “fat tail” events in statistical jargon). In practical terms, it reminds planners to always have a contingency plan.
- Seasonal and other patterns: Within each year, the data (not fully shown in the annual totals) has seasonal swings – winters are typically higher demand than summers, for example. There are also weekly patterns (Mondays are often the busiest day in A&E) and even time-of-day patterns. Advanced models can take these into account. In fact, NHS England has explored advanced forecasting techniques that recognize repeating patterns by week, month, or year. One modern approach uses a Bayesian forecasting tool called Prophet, originally developed by Facebook, which automatically detects seasonal patterns (like winter peaks or holiday dips) in the data. By using such tools, planners can anticipate, for example, that January will likely see more patients than August, and adjust monthly resources accordingly.
- External factors: NHS data can be combined with external data like weather or flu surveillance. For instance, cold weather is known to increase certain emergencies (like cardiac and respiratory problems). A Bayesian model can actually take weather forecasts into account. In one study, researchers developed a hierarchical Bayesian model for short-term hospital demand that included meteorological data – essentially blending weather forecasts with hospital admission data. Their model could predict spikes in emergency admissions more accurately, especially during periods of rapid temperature change (like a sudden cold snap). This is exactly the kind of probabilistic thinking we’re talking about: you take something uncertain (the weather’s impact on health), you incorporate it into the probability of surges, and then you plan resources accordingly (e.g. be ready to open extra beds when a big freeze is forecast).
By feeding all this information into a Bayesian framework, the NHS can create predictive models for A&E demand. These models might output something like: “There is a 60% chance that weekly A&E attendances in the coming month will fall in this range, but a 10% chance of a much higher surge given the current trends.” Armed with such forecasts, decision-makers can allocate budgets in a more nuanced way. It’s not about precision for its own sake – it’s about being prepared. Knowing there’s even a 10% chance of a surge might justify spending on preventative measures (like opening a temporary ward or scheduling backup staff) that you wouldn’t consider if you only looked at the single “most likely” scenario.
Crucially, Bayesian models are continuously learning. As each week’s actual attendance figures come in, the model updates its beliefs about the next week. If a sudden rise is observed, the probabilities shift upward for the coming period, essentially giving an early warning to managers to divert or boost resources. The NHS already collects weekly A&E data in detail – plugging this into an adaptive model could make budgeting more of a living process rather than a once-a-year guess.
Probabilistic Thinking in Action: Examples and Benefits
It’s all well and good to talk theory, but how might this actually improve A&E budgeting and resourcing on the ground? Let’s explore a couple of scenarios and real-world examples:
1. Winter Pressure Planning: Winters are notoriously difficult for the NHS. Cold weather, flu outbreaks, and now Covid surges in some years, all combine to flood A&Es with patients. Historically, the government often ends up injecting emergency funds mid-winter when hospitals are struggling. For instance, heading into the winter of 2024/25, the government announced nearly £450 million of extra investment to expand urgent and emergency care capacity – basically a reactive top-up to help trusts cope with anticipated high demand. A Bayesian approach would aim to make this less reactive and more planned. If models (using data on virus circulation, vaccination rates, etc.) forecast a high probability of a severe flu season, that contingency funding could be baked into budgets from the start. Hospitals could then recruit seasonal staff or set up overflow clinics before corridors are full of beds. In essence, probabilistic planning buys you preparedness. Instead of hoping for the best and scrambling later, you enter winter with a plan for the worst (while still hoping it won’t be fully needed).
A probabilistic plan might say, “There’s a 25% chance this winter’s A&E attendances will exceed last year’s peak by 15%. We will allocate funding for, say, 10 additional temporary beds and associated staff, which we will activate if weekly attendance goes above X threshold.” If the winter turns out mild, maybe that money isn’t all spent – but avoiding a crisis has enormous value. Traditional budgeting might have left no room for those extra beds until an outcry occurs.
2. Resource Allocation Across Regions: Not all A&Es face the same pressures at the same time. Bayesian decision-making can help distribute budget where it’s needed most. Imagine one region’s data shows an earlier start to flu season than elsewhere. A national or regional NHS team could use that evidence to reallocate funding or support dynamically. In a sense, this is like risk pooling: if you have a pot of reserve funds, you release it to the areas with, say, an 80% probability of running into trouble rather than giving every area the exact same uplift regardless of need. The NHS’s current allocation formula already considers population health needs in a broad sense (e.g. areas with older populations or more deprivation get more funds, as they typically have greater demand). Bayesian methods could enhance these formulas by adding a layer of predictive nuance – for example, predicting which specific hospitals are likely to see unusual spikes next quarter based on local data trends. Those hospitals could get a proportionately larger piece of any contingency budget. This dynamic targeting is something a rigid budget system doesn’t do well, but a probabilistic system excels at, because it is always asking “where is the risk highest?”.
3. Improving Efficiency and Avoiding Overcapacity: On the flip side, Bayesian planning isn’t just about throwing more money around “just in case.” It’s also about avoiding waste by calibrating resources to genuine needs. For example, if a model shows only a 5% chance of needing a very high cost measure, managers might decide that it’s not worth funding unless that likelihood increases. One real-world example comes from how hospitals manage their staffing rotas and bed capacity day-to-day. Some A&Es have experimented with forecasting models to predict surges a few days in advance (using anything from historical patterns to Google search trends for symptoms!). If you can predict tomorrow looks quiet with high confidence, you might save money by scheduling one less agency doctor shift – a small but cumulatively significant saving. Conversely, if tomorrow has a high chance of being busy, you call in extra staff proactively (which might cost a bit more upfront but prevents expensive outcomes like patients waiting too long or being put in overflow care). Over a year, these micro-adjustments guided by probability can add up to more efficient use of the budget. Essentially, Bayesian thinking helps fine-tune the balance between too much and too little.
4. Evidence from Research: Academic studies back up the benefits of Bayesian approaches in emergency care. We mentioned a study where a Bayesian model incorporating weather data outperformed the simple methods hospitals often use (like moving averages) in predicting admissions. To put that plainly: hospitals that used a more sophisticated, probability-based model could better anticipate surges than those relying on “last month we had X patients, so next month maybe X+ a bit.” Better anticipation means better allocation of beds, staff, and yes, budget. If you know a surge is likely next week, you might open a temporary ward for that week. If you don’t, you might end up paying overtime, ambulance waiting charges, or other costly consequences of being underprepared. Another example – outside the UK, some health systems use Bayesian decision analysis for staff scheduling. By inputting probabilities of patient arrivals at different times, they create rotas that achieve high service levels with minimal idle time. The same concept could be applied in NHS A&Es to ensure money spent on staffing yields the best coverage at the right times.
Harnessing Bayesian Planning for NHS A&E: Considerations
Moving to a Bayesian-influenced approach for budgeting doesn’t happen overnight. It requires good data, the right tools, and a culture of adaptive planning. The NHS fortunately has the data in spades – not just volumes of patients, but also data on outcomes, costs, and performance. Modern computing makes running complex predictive models feasible even for large systems. NHS analysts can employ techniques like Bayesian networks or Monte Carlo simulations to model A&E demand and costs. In fact, NHS England’s adoption of advanced forecasting tools (such as the Prophet model and others) shows a recognition that these methods can enhance traditional planning.
However, there are a few considerations:
- Uncertainty is uncomfortable. Policymakers and the public are used to hearing definitive plans: “We will do X with Y budget and achieve Z.” Introducing probabilistic thinking – “We are allocating extra funds here because there’s a 30% chance of a surge” – is a shift in mindset. It requires communicating that not all funds might be used, and that’s okay because their allocation is like an insurance policy. This might actually be a positive if communicated well: taxpayers may appreciate that the NHS is planning for contingencies rather than constantly running in crisis mode.
- Defining the utility. Bayesian Decision Theory hinges on what outcome you’re trying to optimize. Is it purely financial (staying within budget)? Is it patient health outcomes (e.g. minimizing waiting times or mortality)? In reality, it’s a trade-off – the NHS wants to stay within budgets and provide excellent care. A Bayesian approach can handle multiple objectives (through assigning utilities or costs to different outcomes), but it works best when you can quantify these. For instance, what “cost” do we assign to a patient waiting over 4 hours in A&E? Not in pounds, but in terms of how much we want to avoid it relative to financial cost. These are ultimately policy decisions that need consensus.
- Continuous learning curve: Implementing Bayesian budgeting would be an iterative process. The first models might not be perfect – they’ll improve over time with refinement and as more data (including data on their own predictions vs reality) becomes available. The NHS would need to invest in analytics capability and perhaps train decision-makers to interpret probabilistic outputs. Instead of a single number forecast, they’ll see ranges and confidence intervals. That’s a positive step, but it requires a bit of statistical literacy at the leadership level.
In conclusion, Bayesian Decision Theory offers a powerful toolkit to improve A&E budget allocation by embracing uncertainty rather than ignoring it. Traditional budgeting often acts like we have a crystal ball (coming up with one forecast and planning around it), whereas Bayesian budgeting acknowledges we have a fuzzy crystal ball – but we can still make optimal decisions by considering the odds of different futures. For the NHS’s A&E departments, this could mean the difference between being caught off-guard by the next surge versus handling it smoothly with resources that were set aside in advance.
The NHS has always been about planning for the worst while hoping for the best. Bayesian methods simply add some mathematical rigor to that credo. By using the wealth of data at hand – from historical attendance figures to real-time indicators – and by updating plans as situations evolve, the NHS can allocate its A&E budgets more adaptively. In plain terms, it means money where and when it’s needed most, and less money wasted where it’s not needed. For patients and staff on the frontline, the impact of better budget planning would be tangible: fewer nights when the A&E is overrun and understaffed, and more confidence that even if tomorrow brings a surprise, the system has a cushion to absorb it.
Bayesian Decision Theory might sound technical, but at heart it’s about smart decision-making in an uncertain world. And in the unpredictable world of A&E healthcare, that could be a real lifesaver – both for lives and for budgets.