The Fuller Stocktake Report, commissioned by NHS England, provides a comprehensive review of the current state of primary care integration within the UK’s healthcare system. The report’s recommendations, which are centred around improving patient care, enhancing workforce capabilities, and strengthening system infrastructure, are underpinned by robust data and analysis.
This article delves into what I think are the data and analysis impacts on the report and the immediate data provisions which will be and have been instrumental in shaping these recommendations.
Data-Driven Personalised Patient Care
The report emphasises the need for a more personalised approach to patient care. The recommendation for the development of a ‘Personalised Care and Support Plan’ (PCSP) for every patient is based on data showing that personalised care can significantly improve patient outcomes and satisfaction. The data analysed in the report includes patient feedback, clinical outcomes, and patient engagement levels, all of which point towards the benefits of a personalised approach. This data-driven recommendation ensures that the proposed PCSPs are not just theoretical concepts, but are grounded in empirical evidence.
Digital Health Services Expansion
The report’s advocacy for the expansion of digital health services is another recommendation that is rooted in data. The data analysed includes patient satisfaction rates with online consultations, usage rates of digital health services, and the impact of digital health interventions on patient outcomes. The analysis of this data provides a compelling case for the expansion of digital health services, demonstrating that they can offer a convenient and effective alternative to traditional face-to-face services.
Workforce Development and Collaboration
The report identifies the enhancement of the primary care workforce’s capabilities as a key priority. The recommendation for the implementation of a ‘Workforce Development Plan’ is supported by data showing that workforce development can lead to improved patient care and increased staff retention. The data analysed includes staff turnover rates, patient satisfaction scores, and the impact of training programmes on staff performance. This data-driven approach ensures that the proposed Workforce Development Plan is tailored to the specific needs and challenges of the primary care workforce.
The report’s recommendation for the establishment of ‘Primary Care Networks’ (PCNs) is also based on robust data and analysis. The data analysed includes the impact of collaboration and knowledge sharing on patient care and resource utilisation. The analysis of this data demonstrates that PCNs can lead to improved patient care and more efficient use of resources, providing a strong case for their establishment.
Strengthening System Infrastructure
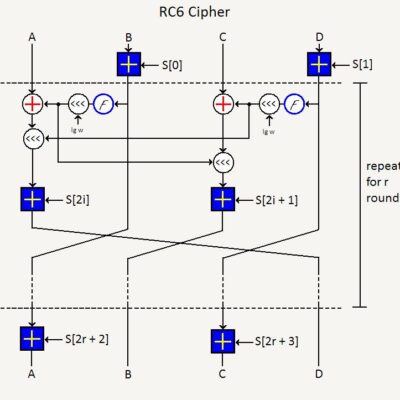
The report underscores the importance of robust system infrastructure in supporting primary care integration. The recommendation for the development of a ‘Digital First’ approach is supported by data showing that digital technology can significantly enhance the delivery of healthcare services. The data analysed includes the impact of digital technology on operational efficiency, patient satisfaction, and patient outcomes. This data-driven approach ensures that the proposed ‘Digital First’ approach is grounded in empirical evidence and is likely to deliver tangible benefits.
The report’s advocacy for the strengthening of governance structures is another recommendation that is underpinned by data and analysis. The recommendation for the establishment of a ‘Primary Care Integration Board’ is based on analysis suggesting that strong governance can facilitate the successful integration of primary care services. The analysis includes case studies of successful governance structures, the impact of governance on organisational performance, and the role of governance in facilitating change. This data-driven approach ensures that the proposed governance structures are likely to be effective in supporting primary care integration.
Some immediate data driven actions that can support this approach could include :
- Implement Real-Time Data Tracking: One of the first steps a data team can take is to implement real-time data tracking across all primary care services. This will allow for immediate access to patient data, enabling healthcare professionals to make informed decisions swiftly. Real-time data tracking can also help identify trends and patterns, allowing for proactive measures to improve patient care.
- Develop Predictive Models: Using historical data, the team can develop predictive models to forecast future healthcare needs. These models can help anticipate patient needs, allowing for better resource allocation and planning. For instance, predictive models can help identify potential health risks in a population, enabling early intervention and prevention strategies.
- Enhance Data Visualisation: Data visualisation tools can help transform complex data sets into understandable and actionable insights. By developing interactive dashboards and reports, the data team can provide healthcare professionals with a clear view of patient data, trends, and patterns. This can support decision-making processes and improve the overall efficiency of primary care services.
- Implement Data Governance: To ensure the quality and reliability of data, it’s crucial to implement robust data governance practices. This includes establishing clear policies and procedures for data management, ensuring data accuracy, and promoting data security. Effective data governance can enhance the trustworthiness of data-driven insights and support informed decision-making.
- Integrate Data Sources: Often, valuable patient data is spread across multiple systems and databases. By integrating these data sources, the data team can create a more comprehensive view of patient health and care. This integrated approach can support more personalised care plans, improve coordination among healthcare providers, and ultimately enhance patient outcomes.
The Fuller Report’s recommendations are firmly grounded in robust data and analysis. This data-driven approach ensures that the proposed changes are not just theoretical concepts, but are likely to deliver tangible benefits for patients, healthcare professionals, and the healthcare system as a whole. As the UK healthcare system continues to evolve, the insights and recommendations presented in this report, underpinned by robust data and analysis, will undoubtedly play a crucial role in shaping its future direction.